Splanchnic Nerve Block and Radiofrequency Ablation-Dr Debjyoti Dutta
- Dr Debjyoti Dutta
- Apr 20, 2024
- 9 min read
A different method to the paravertebral (retro-crural) coeliac plexus approach is the Splanchnic Nerve Block technique introduced by Abram and Boas. This technique involves blocking the branches of the Splanchnic Nerve derived from the thoracic sympathetic trunk, thereby interrupting the nerve supply to the coeliac plexus.
Advantages of Splanchnic Nerve Block over Coeliac Plexus Block for Upper Abdominal Pain
Precision: Targets the splanchnic nerves from the thoracic sympathetic trunk, avoiding unwanted effects on nearby structures.
Radiofrequency Neurotomy: Possible at the splanchnic level, providing longer pain relief than neurolytic blocks. Radiofrequency Neurotomy is not possible at the coeliac level due to the large size of the plexus.
Reduced Side Effects: Less likely to affect adjacent structures or cause complications by selectively blocking the splanchnic nerves.
Lower Volumes of Medication: Achieves effective pain relief with lower doses of medication, reducing systemic side effects.
Ease of Procedure: Easier and less invasive than some techniques used for coeliac plexus block, especially in complex cases.
Patient Comfort: Increases patient comfort during and after the procedure by minimizing interference with surrounding structures.
Advantages of splanchnic nerve block over coeliac plexus block for the management of upper abdominal pain
| ||
Advantage | Splanchnic Nerve Block | Coeliac Plexus Block |
Precision in Targeting Nerves | High | Low |
Radiofrequency Neurotomy | Possible | Not possible |
Reduced Side Effects | Likely | Unlikely |
Pain Relief with Lower Volumes of Medication | Yes | No |
Ease of Procedure | Easy | Difficult |
Patient Comfort | High | Low |
Anatomy Splanchnic Nerves -
The splanchnic nerves are comprised of medial branches from the T5 to T12 sympathetic ganglia.
The greater splanchnic nerve - derived from T5–T9 ganglia. (Variation T5–T10)
The lesser Splanchnic Nerve - derived from T10 – T11 ganglia. (Variation T9–T10, T10–T12, T10–T11)
The Lesser Splanchnic Nerve - derived from T12 ganglia
The greater splanchnic nerves descend in the paravertebral space, obliquely, giving off branches to the descending aorta and perforating the crus of the diaphragm
The greater splanchnic nerve synapses in the superior aspect of celiac ganglia
Innervates: Gastrointestinal tract (from distal oesophagus to mid-transverse colon) pancreas, stomach, liver, adrenals, ureters, abdominal vessels
Indications of Splanchnic Nerve Block
Indications of Splanchnic Nerve Block are as follows.
Cancer Pain: Splanchnic nerve blocks are frequently utilized for pain management in diverse abdominal malignancies, such as pancreatic malignancy, hepatocellular carcinoma in liver malignancy, and gastric malignancy. These blocks are applied to effectively address abdominal pain associated with gallbladder malignancy and splenic malignancy, including splenic lymphoma or other malignancies affecting the spleen. Additionally, splanchnic nerve blocks are considered for pain relief in adrenal gland malignancies like adrenocortical carcinoma. In the context of metastatic abdominal malignancies spreading to various organs.
Pain Due to Chronic Pancreatitis - Usually Radiofrequency Ablation of splachnic nerve is preferred in non-malignant cases.
Differential diagnosis of somatic versus visceral pain: This is a pain that helps to distinguish between pain originating from the skin, muscles, bones, or joints (somatic pain) and pain originating from the internal organs (visceral pain). Somatic pain is usually well-localized, sharp, and aggravated by movement, while visceral pain is usually diffuse, dull, and associated with nausea, vomiting, or changes in bowel habits.
Treatment of patients who have failed to obtain relief from celiac plexus blocks: This is a pain that occurs when the celiac plexus, a network of nerves that innervates the upper abdominal organs, is damaged or compressed by tumours, inflammation, or surgery. Celiac plexus blocks involve injecting a local anaesthetic or a neurolytic agent near the celiac plexus to block the pain signals. However, some patients may not respond well to this procedure, and may benefit from splanchnic nerve blocks instead.
Palliation of the acute pain of arterial embolization of the liver for cancer therapy: This is a pain that occurs when a catheter is inserted into an artery that supplies blood to the liver, and small particles are injected to block the blood flow to the tumour. This can cause ischemia and necrosis of the liver tissue, resulting in severe pain. Splanchnic nerve blocks can help to reduce the pain and improve the quality of life of the patients undergoing this treatment.
Treatment of pain of abdominal “angina” associated with visceral arterial insufficiency: This is a pain that occurs when the blood supply to the abdominal organs is reduced due to atherosclerosis, thrombosis, or vasospasm of the visceral arteries. This can cause intermittent episodes of severe abdominal pain, similar to angina pectoris of the heart. Splanchnic nerve blocks can help to relieve the pain and prevent further ischemic damage to the organs.
Contraindications for Splanchnic Nerve Block:
Splanchnic Nerve block is contraindicated in the following conditions
Infection at the Injection Site: - Splanchnic nerve blocks should be avoided if there is an active infection at the injection site or in the surrounding area.
Bleeding Disorders: - Patients with bleeding disorders or those taking anticoagulant medications may be at an increased risk of bleeding complications, and therefore, splanchnic nerve blocks should be approached with caution.
Allergy to Local Anaesthetics or Contrast Agents: - Individuals with a known allergy to the local anaesthetics or contrast agents used in the procedure should not undergo splanchnic nerve blocks.
Unstable Cardiovascular Status: - Patients with unstable cardiovascular conditions may not be suitable candidates for splanchnic nerve blocks due to the potential hemodynamic effects of the procedure.
Severe Pulmonary Disease: - Individuals with severe pulmonary disease may be at an increased risk of respiratory complications during the procedure, making splanchnic nerve blocks contraindicated in such cases.
Inadequate Patient Cooperation: - The procedure requires patient cooperation and the ability to maintain a suitable position during the injection. Patients who cannot tolerate the necessary positioning or cooperate during the procedure may not be suitable candidates.
Spinal Abnormalities or Anomalies: - The presence of spinal abnormalities or anomalies may make it technically challenging to perform splanchnic nerve blocks safely.
Pregnancy: - Splanchnic nerve blocks are generally avoided during pregnancy, especially in the early and late stages, due to potential risks to the foetus.
Local Skin Infections: - If there is an active skin infection at the site of injection, it is advisable to postpone the splanchnic nerve block until the infection has resolved.
Procedure -
Equipment and Monitoring
Conducting a safe and effective splanchnic nerve block necessitates a well-equipped procedural setup. Standard ASA monitors are essential for continuous patient monitoring, ensuring vital signs are closely observed throughout the procedure. The utilization of a C-arm facilitates real-time imaging, enhancing precision in needle placement. A sterile environment is maintained through thorough preparation and draping. Prior to any needle larger than 25G, skin local anaesthesia is administered unless sedation is employed for patient comfort. Specific needles are employed based on the nature of the intervention: a 22G, 15 cm needle with a curved tip for diagnostic injections, and an 18–20G, 15 cm curved-tip radiofrequency cannula with a 10 mm active tip for radiofrequency ablation (RF). A grounding pad is utilized to ensure electrical safety during RF procedures. The RF generator, equipped for unipolar and bipolar lesions, is crucial for the precision and effectiveness of the ablation. To maintain patient hydration and support hemodynamic stability, a preprocedural infusion of 500 ml fluid is administered. Local anaesthetic agents contribute to pain management during the procedure. Additionally, the use of a non-ionic contrast agent, such as Iohexol, aids in visualizing the target area, ensuring accurate needle placement. This comprehensive array of equipment and medications underscores the importance of a well-prepared and meticulously executed approach to splanchnic nerve blocks, optimizing patient safety and procedural success.
Equipment and monitoring required for splanchnic nerve block.
Equipment | Description |
Standard ASA monitors | To monitor vital signs such as blood pressure, heart rate, oxygen saturation, etc. |
C Arm | To provide fluoroscopic guidance for needle placement |
Sterile prep, and drape | To prevent infection and maintain asepsis |
Skin local anaesthesia | To numb the skin and reduce pain from needle insertion |
22G, 15 cm needle | To inject local anaesthetic near the splanchnic nerves for diagnostic purposes |
18–20G, 15 cm curved tip radiofrequency cannula | To deliver radiofrequency current to the splanchnic nerves for ablation |
Grounding pad | To complete the electrical circuit and avoid burns |
RF generator | To generate and control the radiofrequency current |
Infusion of 500 ml fluid | To prevent hypotension and dehydration |
Local anaesthetic | To block the transmission of pain signals from the splanchnic nerves |
Non-ionic Contrast Agent (Iohexol) | For Confirmation of Final Needle Position |
Patient Positioning - The patient is lying in prone position with support under the abdomen to achieve thoracolumbar kyphotic position.
Method -
The T11 vertebral body is identified, after which the C-arm is rotated from the anteroposterior orientation in a caudal and lateral direction, allowing the concave mid-portion of the vertebral body to be visualized without being obscured by ribs or the transverse process.
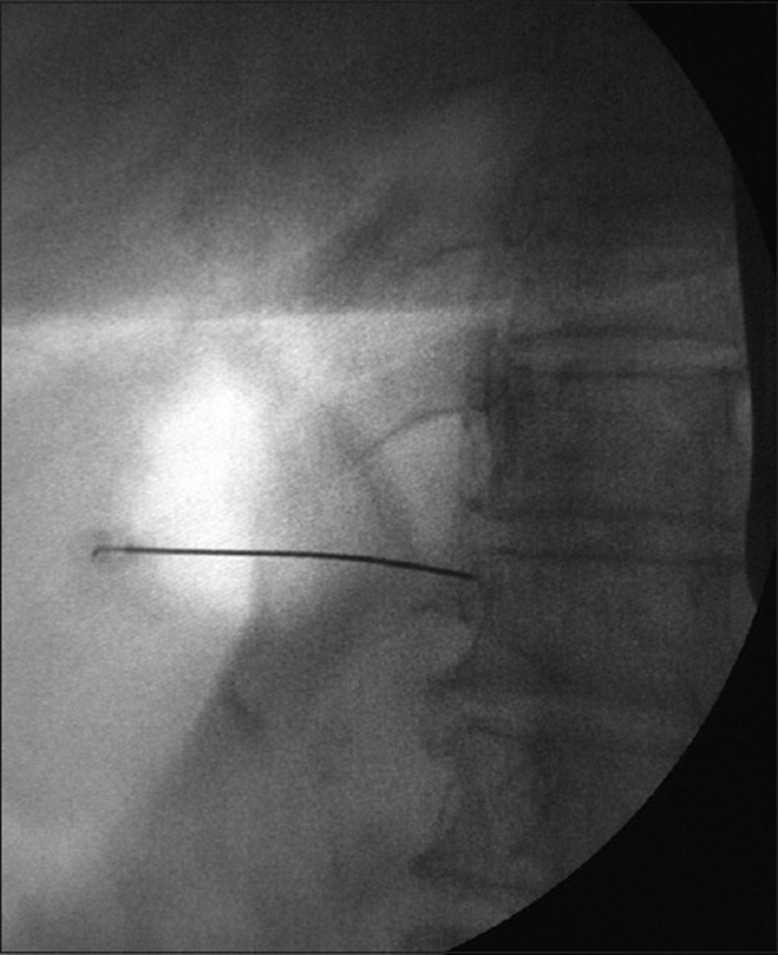
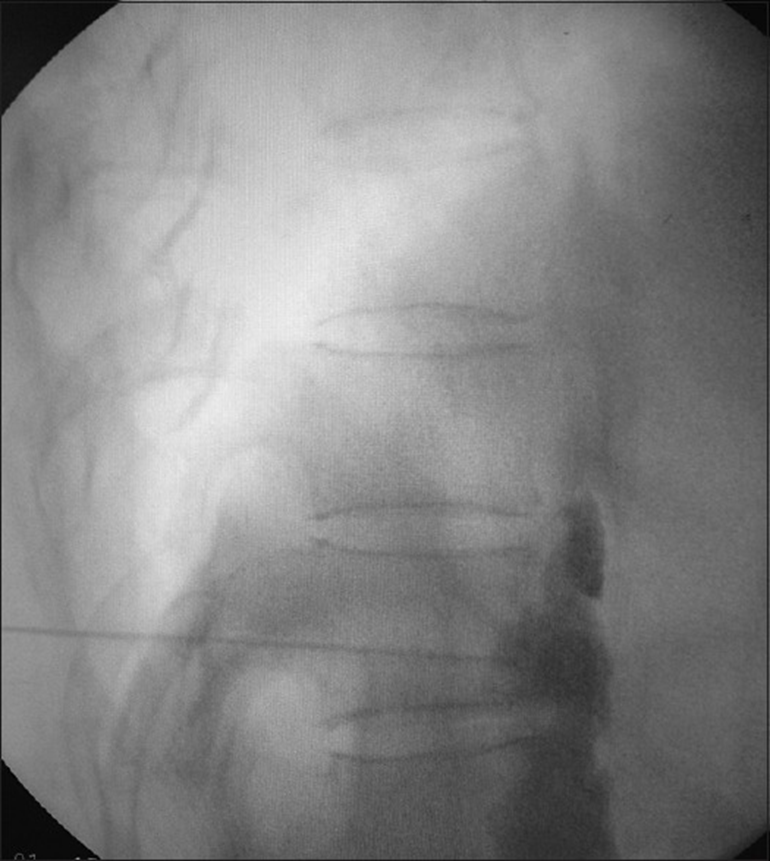
A 20 or 22G, 15 cm needle is inserted paravertebrally, using a tunnel view, in the direction of the concave mid-portion of the vertebral body. Try to make contact with the vertebral body. Under lateral fluoroscopy, the needle is advanced to the anterolateral aspect of the T11 vertebral body at the junction of anterior 1/3rd and Posterior 2/3rd in the lateral view. Radiographic imaging should show the tip of the needle just within the contour of the T11 body in an anteroposterior view and at the junction of anterior 1/3rd and Posterior 2/3rd in the lateral view.
A small volume of contrast medium is injected to check dispersion along the anterolateral aspect of the vertebral body.
For Diagnostic Injection - 10-15 ml of lidocaine (0.5-2%) or 10-15 ml of bupivacaine (0.125-0.25%) are injected in divided doses after negative aspiration to rule out intravascular injections.
Injection of Neurolytic - Before the neurolytic agent is injected (as described above), the area around the needle is covered with wet gauze, after which the neurolytic solution can be injected in fractions, preferably together with contrast medium. The volume of injectate is usually 25 ml on each side but can range between 16-80 ml. The volume is dependent on the positioning of the needle and the ease of flow in the area. The needles then have to be flushed with saline, or a local anaesthetic before withdrawing.
For RF Lesioning - After sensory and motor stimulation, 2 ml of lidocaine 2% is injected before ablation. After Sensory and Motor Stimulation, RF Lesioning is done at 80 Degrees C for 90 seconds and is repeated after rotating the needle 180 degrees.
The same procedure is repeated on the other side.
After the procedure, patients may experience pain at the insertion site,
Orthostatic hypotension or diarrhoea. Patients should therefore be sufficiently hydrated and hospitalized for a night to check for signs of hypotension.
The anteroposterior view of the needle position in the splanchnic nerve block
The Lateral view of the contrast spread in the splanchnic nerve block.
The lateral view of the needle position in the splanchnic nerve block
Post-Procedure Instructions Following a Splanchnic Nerve Block
§ Post-procedure care following a splanchnic nerve block is crucial to ensure the patient’s well-being and maximize the benefits of the intervention. While specific instructions may vary depending on individual patient characteristics and the nature of the procedure, the following general post-procedure guidelines are often recommended:
§ Observation Period:
o Patients are typically monitored for a short period in a recovery area to assess vital signs, any immediate adverse reactions, and the initial response to the procedure.
§ Rest and Recovery:
o Patients are advised to take it easy for the remainder of the day following the procedure. Activities that involve strenuous physical exertion or heavy lifting should be avoided.
§ Pain Management:
o It’s common to experience some soreness or discomfort at the injection site. Paracetamol or NSAIDS used for post procedure pain.
§ Hydration:
o Adequate hydration is encouraged post-procedure. Patients are advised to drink plenty of fluids.
§ Monitoring for Adverse Effects:
o Patients should be vigilant for any signs of infection at the injection site, increased pain, or unusual symptoms and promptly report them to their doctor.
§ Gradual Resumption of Activities:
o While rest is recommended initially, patients can gradually resume normal activities in the days following the procedure.
§ Follow-Up Appointment:
o A follow-up appointment may be scheduled to assess the effectiveness of the procedure and address any concerns or questions the patient may have.
§ Documentation of Effects:
o Patients are often encouraged to keep a pain diary, documenting changes in pain levels and any associated symptoms following the splanchnic nerve block.
§ Contact Information:
o Patients should have clear instructions on whom to contact in case of emergency or if they have questions or concerns post-procedure.
Individualized care and attention to patient needs contribute to a successful recovery following a splanchnic nerve block.
Complications of Splanchnic Nerve Block -
Splanchnic nerve blocks, while generally considered safe and effective, are associated with rare complications that healthcare providers must be vigilant about. The incidence of these complications is relatively low, emphasizing the procedure’s overall safety when performed by skilled practitioners. It is crucial for both clinicians and patients to be aware of these potential adverse effects to ensure informed decision-making and prompt management if complications arise.
Hypotension: may occur following the procedure. While uncommon, clinicians monitor patients closely for this possibility, taking swift action if necessary to stabilize blood pressure.
Pneumothorax: An infrequent complication that underscores the importance of precise needle placement to avoid unintended puncture of the pleura, and careful patient monitoring post-procedure.
Chylothorax: An exceptionally rare but recognized complication.
Acute alcohol intoxication symptoms: May manifest in some cases. This highlights the need for patients to disclose their medical history, including alcohol consumption, to ensure proper risk assessment and management.
Infection: A rare but serious complication that healthcare providers guard against through stringent aseptic techniques. Monitoring for signs of infection post-procedure is crucial for early detection and intervention.
Paraesthesia: may occur due to nerve irritation during the procedure. Although transient in most cases, clinicians remain attentive to patient comfort and address any persistent paraesthesia.
Nerve damage: A rare potential concern,
Vascular injection and damage: Rare but serious complications, underlining the necessity of precise needle placement and continuous monitoring to identify any vascular-related issues promptly.
Epidural or subarachnoid injections: A potential complication that underscores the importance of accurate needle placement to avoid unintended spinal cord exposure.
Organ puncture: A rare but recognized complication.
Drug allergies: May manifest as an uncommon complication, necessitating thorough pre-procedural screening for any known allergies to medications used during the splanchnic nerve block.
In conclusion, while complications associated with splanchnic nerve blocks are rare, patients must be aware of these potential adverse effects. A thorough understanding of the risks and benefits, coupled with skilled procedural techniques and vigilant post-procedural monitoring, ensures the overall safety and success of splanchnic nerve block.




Comments